Vascular Conditions and Treatments
Our legs and feet work really hard throughout our life: getting us up in the morning, bringing us to work every day, standing while cooking, walking up the mountains or through that gym class. Without the health of the blood vessels, we would find our lives less active, our mobility considerably reduced and possibly experience pain or limb-threatening conditions. Problems with the vessels in the lower leg can happen at any age but are more common at more mature stages of our lives.
To help prevent conditions of the lower limb vessels and treat current complaints it’s helpful to first understand what are the main vessels in the legs, how do they work and what happens when they become damaged and no longer work as they should.
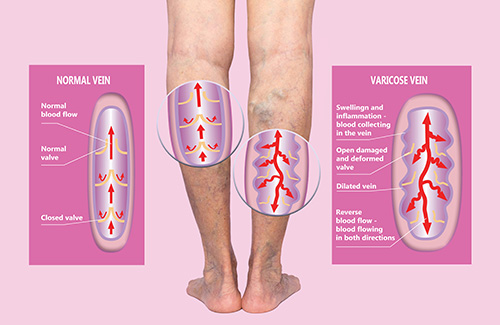
The venous system is a complex network of superficial and deep veins in which deoxygenated blood is conveyed from the periphery to the heart. This is a low-pressure system that relies on venous valves and muscle contraction (foot dorsi-flexion and calf muscle pump) to return blood to the heart against the gravity.
The Long (or Great) Saphenous – LSV and the Short Saphenous Vein – SSV are the main superficial veins of the legs; the Anterior Thigh Vein, the Giacomini and the Intersaphenous Veins are also important tributaries. The superficial veins drain into the deep venous system via junctions in the groin (sapheno-femoral) and behind the knee (sapheno-popliteal) and small perforator veins crossing the muscles.
Varicose veins are chronically dilated and tortuous superficial veins with reversed blood flow due to incompetent damaged valves and/or diseased venous wall. The stasis of the blood (venous hypertension) in the lower extremities may lead to chronic swelling, skin changes (pigmentation, eczema) and ultimately the risk of developing ulcerations. Often varicose vein may bleed or cause localised painful inflammatory process (phlebitis).
Risk factors for developing varicose veins include predisposition/family history, previous injuries, fractures or deep vein thrombosis – DVT (post thrombotic syndrome). The prevalence rises with age and often develop or deteriorate during pregnancy.
You may be have an increased risk of developing varicose veins if:
- You are pregnant or have had multiple pregnancies
- Stand for long periods of time at work or have a sedentary life-style
- Are overweight for your height
- Have reduced movement or ankle joint or calf muscle waist
- Have a family history of varicose veins
Stages of Venous Disease
- Spider Veins
Spider veins or Telangiectasia are tiny, dilated blood vessel capillaries arising from a central point therefore resembling a spider web. They can occur near the surface of the skin. Spider veins can be perceived as a cosmetic condition and have no clinical implication;

- Reticular Veins
Reticular veins are varicosities 1-3 mm in diameter; they can be an early sign of venous disease and it is useful to have them checked out along with any other symptoms you may be experiencing in your legs such as:
- pain, itchiness, leg heaviness
- skin changes such as dark, brownish pigmentation or eczema
It is reassuring to note that if the early sign of venous disease are addressed in the proper way it can prevent further complications later in life.

- Truncal Varicose Veins
Varicose veins 4mm or larger are defined as truncal; these are usually involving the long or short saphenous veins and the main tributaries. Truncal reflux may lead to venous hypertension and is associated to the risk of developing venous leg ulcers

- Oedema
More commonly known as swelling, it is usually located at the ankles, feet or legs. Oedema is a build-up of fluid. This can be very uncomfortable and may leave your legs feeling heavy and in some cases aching. It is important to investigate whether incompetent veins or lymphatic vessels (often a combination of the two) are causing the congestion. The good news is that venous-lymphatic oedema can be alleviated by appropriate support stockings/socks or compression hosiery and with elevation, rest and lifestyle advice
- Pigmentation or eczema
Haemosiderin staining is a typical clinical sign that you may have moderate to severe venous insufficiency. This is easy to recognise and to check yourself.
Usually located on the lower part of the leg or possibly the ankle, venous staining often presents as a notably brown, rusty yellow or black skin discolouration. This happens when the haemoglobin in the red blood cells leak out of the superficial veins as the result of the venous stasis.
It is usually not painful but can make the skin drier, frailer more susceptible to breakdown and possibly ulceration.

- Lipodermatosclerosis or athrophie blanche
Lipodermatosclerosis or athrophie blancheis is a form of chronic inflammation of the fat under the skin resulting into thickening, hardening and colour changes of the skin.
- Healed venous ulcer
C5 in the CEAP classification of chronic venous disease (link with photo). The risk of recurrences is extremely high unless the underlying venous hypertension is treated.
- Active venous ulcer
An active venous ulcer is classified as C6 in the CEAP classification of chronic venous disease (link with photo). Leg ulcer are a physical, psychological and economic burden. They may impact on your personal and social life. The correct treatment should include a holistic management by means of:
- appropriate wound care
- compression therapy
- surgical or endovenous treatment of the underlying truncal reflux
Management
The management of varicose veins, depending on the stage of the disease, your anatomy and your personal preference (following thorough informed discussion) may include:
- lifestyle recommendations and skin care
- Maintaining a healthy weight
- Eating a well-balanced and healthy diet
- Exercising
- Moving – if you sit or stand for long periods of time make sure to get up and move regularly
- Elevating your feet and legs above heart level – this can have a real soothing effect after a long day
- looking after and moisturising your skin
- interventional treatments of the varicose veins
- “key hole”, minimally invasive, endothermal ablation (radiofrequency – RFA)
- ultrasound guided foam sclerotherapy
- surgical avulsions and/or ligations of perforator veins
- fitted or customised compression hosiery
- Wearing fitted or customised compression hosiery or socks/stockings to support your veins
- the appropriate combination of the above
When attending the Vascular Clinic, a comprehensive anamnesis (personal and medical history) and a physical examination will be performed.
A duplex ultrasound scan may be arranged to further investigate the deep and superficial venous systems, the level of venous reflux and to map your varicose veins with the view of identifying the most suitable treatment strategy.
Mr Biasi will discuss with you how well each treatment is likely to work and the possible limitations or side effects.
If neither endothermal ablation nor ultrasound-guided foam sclerotherapy are suitable for you, you should be offered surgery. This is usually a type of surgery called ligation and stripping, in which the varicose vein is tied off and then removed

Thermal Ablation

Surgical Avulsions
Sclerotherapy
Thermal Ablation
The arteries carry oxygenated, high-pressure blood and nourishment from the heart to the organs and tissues of the body.
The Aorta represents the main trunk of the “arterial tree”, originating from the left ventricle of the heart; the main distribution branches in the pelvis and lower limbs are named iliac, common femoral, profunda femoris, superficial femoral, popliteal and tibial arteries reaching the foot.
In healthy, elastic vessels the arterial pulse can be felt over the arteries when lying near the surface of the skin as the result of the pumping action of the heart.
A blockage in the peripheral arteries may lead to a dramatic deterioration of the blood supply, affecting the nerves, muscles and skin of the limbs. This may occur as a sudden event (acute ischaemia) or as a chronic build-up of fat, cholesterol, platelets (“atheromatous plaque”) slowly narrowing the arterial lumen (peripheral arterial disease – PAD) progressively reducing the blood flow and pressure until reaching a complete, irreversible blockage.
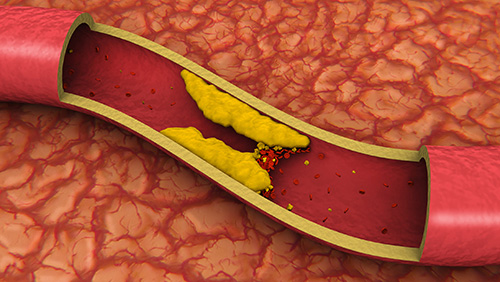
Smoking, high blood pressure, high cholesterol are some of the predisposing conditions that can be reduced with life-style modification and best medical therapy; male gender, age and genetic predisposition are unfortunately non-modifiable risk factors.
Classification
PAD may present with a wide spectrum of signs and symptoms:
- intermittent claudication: leg muscles cramp-like pain that triggers when walking a certain distance (the etymology of the name “claudication” comes from the ancient Roman emperor Claudius who reportedly was limping)
- rest pain: constant, debilitating leg pain; often keeps you awake at night-time. The only relief is to hang your leg off the bed or to sleep on the chair
- leg ulcerations: non-healing, arterial ulcers; these are prone to get infected and to evolve into a limb-threatening gangrene
Intermittent claudication (IC) is often a benign condition and the first-line management should be conservative by means of structured walking exercise and secondary cardiovascular risk factors modification. However, IC may sometimes progress into severely impairing walking limitations affecting the overall physical and psychological well-being.

A thorough vascular assessment is paramount to reach a correct differential diagnosis which should include:
- arterial claudication
- venous claudication
- neurological claudication
- muscle and joint claudication (musculoskeletal)
Ischaemic rest pain and foot-leg ulcerations are severe limb-threatening conditions (often referred as Critical Limb Ischaemia – CLI); timely diagnosis and intervention are indispensable to save the limbs from the risk of irreversible functional damages, life-threatening blood stream infections and limb loss.
The vascular assessment will comprise of:
- anamnesis (personal and medical history)
- comprehensive physical examination
- Doppler test (static or dynamic measurement of the pressure in the arteries of the leg)
- Ultrasound Duplex scan to investigate the anatomy of the vessels and to identify the extent and severity of the blockage or flow-limiting narrowing
- second level imaging (e.g. CTA, MRI) for differential diagnosis or surgical planning
Medical and Surgical management (according to the stage and anatomical distribution of the disease):
- life style recommendations
It is important to consider your lifestyle as part of your overall treatment plan to help support prevention, optimal treatment outcomes and recovery, and avert recurrences.
We are here to support and discuss with you how this may impact on your health and the overall benefits to your wellbeing.
Areas to consider:
- Diet and how it can be optimised to reduced lipid intake
- Exercise and how to improve joint and muscle functions and to promote collateral circulation
- Skin and nail care
- Footwear
- Smoking cessation strategies
- structured walking exercise programme (for IC)
- best medical therapy – medications
- minimally invasive “key-hole” endovascular treatment
- angioplasty and stenting (drilling through the plaque and stretching open a channel in the blocked arteries)
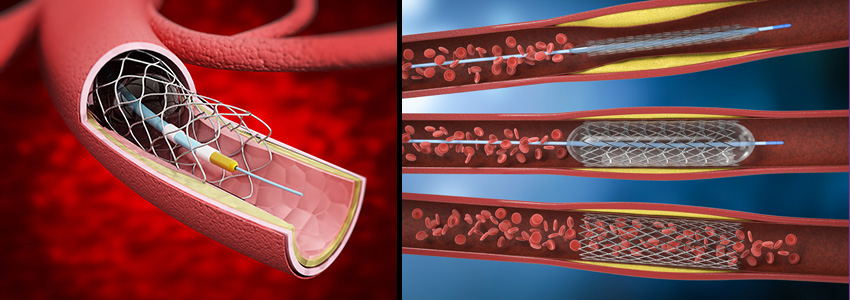
- atherectomy and shockwave intravascular lithotripsy (cutting edge technologies to debulk the plaque and to re-open heavily calcified, hardened arteries without the need of permanent metal stents)
- angioplasty and stenting (drilling through the plaque and stretching open a channel in the blocked arteries)
- open bypass surgery
- using a superficial vein as a conduit to bypass the blockage
- durable and preferable in young, fit patients
- hybrid procedures
- the combination of concomitant open surgery and endovascular therapy, performed in the state-of-the-art “hybrid theatre”. If suitable, this approach may offer the best outcomes
Surgical and endovascular treatments requires a close ultrasound and clinical surveillance, together with strict adherence to individualised medication strategies in order to optimise long-term results
Diabetic patients are exposed to the risk of developing foot complications in the form of ulcerations, infection and/or destruction of the deep tissues, associated with neurological abnormalities and various degrees of peripheral vascular disease in the lower limb.
The prevalence of foot ulcerations in patients with diabetes who live in developed countries has been reported as high as 10%; type 2 diabetes, older age, pre-existing neuropathy, reduced joint mobility and increased foot pressures are considered risks factors.
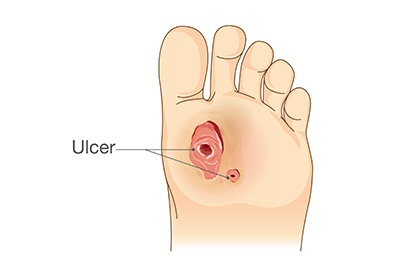
The Diabetic Foot is a complex, multifactorial condition; the main determinants and prognostic elements are highlighted in the WIfI classification:
- extension of the Wound
- Ischaemia / impaired circulation
- Foot Infection
Diabetic foot ulcerations must be dealt as medical and surgical emergencies, due to the impending risk of rapidly evolving bloodstream infection (sepsis) and the risk of limb loss (minor or major amputations), potentially leading to devastating sequelae on the person’s psycho-physical condition and quality of life.
Assessing and restoring adequate blood perfusion (see PAD section), controlling the infection and diabetes, adequate wound & foot care are the therapeutic pillars. This requires the multidisciplinary joint expertise of Vascular Surgeons, Diabetes Physicians, specialist Podiatrists and Infectious Disease Doctors.
The carotid arteries are the main arterial vessels (together with the vertebral arteries) providing blood flow and oxygen to the brain.
Atheromatous disease of the carotid wall (chronic fatty-deposits called “plaques”) may lead to the narrowing of the arterial lumen and/or to thromboembolic cerebrovascular accidents (CVA: TIA and Stroke).
Transient Ischaemic Attacks – TIA and Stroke may occur when the blood supply to the brain is severely impaired. An embolus (a clot or piece of plaque breaking off) can flow to and block the smaller arteries depriving your brain of oxygen. This leads to either transitory (TIA) or permanent (Stroke) damages. Stroke is the most common cause of death and the leading cause of permanent disability.
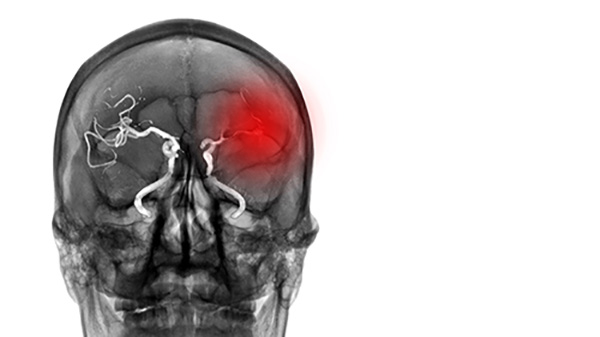
The main causes (aetiology) of a stroke or TIA are:
- carotid disease
- irregular heartbeat (atrial fibrillation)
- brain haemorrhage
Carotid artery disease may developed slowly and unnoticed for many years until a plaque breaks off leading to a sudden blockage of the carotid or embolic event in the brain.
Signs and symptoms of a stroke or TIA include:
- acute onset of numbness or weakness in the face or limbs, often on one side only of the body (hemiparesis)
- face droop
- slurred speech
- blurred vision and / or trouble seeing in one or both eyes
Urgent referrals to the Stroke Physician and to the Vascular Surgeon are recommended.
Investigations:
- anamnesis and physical examination
- brain scan (diffusion weighted MRI or CT)
- carotid imaging (Duplex and CTA)
- heart imaging (ECG, Echocardiogram)
Management:
- Best Medical Therapy
- (combination of two antiplatelet agents + statin)
- oral anticoagulation (if cardio-embolic)
- Carotid Surgery
The first carotid surgical reconstruction to treat intermittent attacks of hemiplegia was performed at St Mary’s Hospital, London in 1954.
The aim of surgery in people who have recently experienced a carotid stroke is to clear the carotid artery with the view of preventing further embolic events, as recurrences are highly likely to occur within the first month from the index event.
Men younger than 75 years of age would benefit from preventive carotid surgery (asymptomatic), should they present a plaque narrowing the carotid artery for more than 70% of the lumen.
Women have a lower risk of cerebrovascular accidents; hence, asymptomatic surgery is usually not considered beneficial.
Surgical techniques:
- carotid endarterectomy (CEA) and patch plasty
- eversion endarterectomy (eCEA)
- carotid stenting (in selected patients only)
Aneurysm is defined as an enlargement of a vessel greater than 50% of its nominal size.
The Aorta is the main artery originating from the heart and running in the chest and abdomen; trunks to the brain, the upper and lower limbs and visceral branches to the main organs originate from the aorta.
Abdominal Aortic Aneurysm (AAA) occurs when the arterial wall weakens reaching a diameter >30mm.
Causes
- genetic predisposition
- trauma (e.g. causing a tear in the arterial wall – dissection)
- infection (“mycotic aneurysm” – rare)
Risk factors
- smoking, hypertension
- male gender
- family history
Aortic aneurysms often grow slowly without symptoms. AAA are often found during an examination for another reason or during routine medical tests, such as an ultrasound of the heart or abdomen. Some aneurysms expand over time, others quickly. The main risk is the sudden burst of the aneurysm (rupture) which leads to a life threatening internal bleed.
In England, Ultrasound Duplex screening for AAA is offered to men during the year they turn 65: https://www.nhs.uk/service-search/other-services/Abdominal-aortic-aneurysm-screening/LocationSearch/1910
However, Duplex should be recommended to women and men aged 50, if they have a family history of AAA in first degree family members.
Indications for treatment
- non symptomatic AAA larger than 55mm
- non symptomatic AAA larger than 4.0 cm and quickly-growing (more than 1 cm in one year or 5mm in six months)
- symptomatic aneurysm (impending rupture: severe abdominal pain, stabbing back pain)
Investigations
- physical examination
- imaging (Duplex and CTA)
- Cardio-Pulmonary Exercise Test (CPET) to assess pre-operative fitness
Treatment
- Endovascular Aneurysm Repair (EVAR)
- Open Aortic Surgery
Popliteal Artery Aneurysms (PAAs) are the most frequent peripheral aneurysms (defined as pathological enlargement of the artery, > 1.5 times larger than its normal diameter).
PAAs are often bilateral and may present with a coexistent abdominal aneurysm (AAA).
Most PAAs are asymptomatic and diagnosed incidentally. However, they carry a significant risk of acute thromboembolic complications (sudden blockage of the leg arteries), potentially leading to catastrophic ischaemia (irreversible nerve damage and limb loss).
Non-symptomatic PAAs larger than 2.5cm and with significant burden of clot (thrombus) are at risk of future complications and should be considered for preventive treatment. The North American ACC-AHA guidelines recommend to treat asymptomatic popliteal aneurysm > 2cm (Class 1 – Level B evidence). All symptomatic aneurysms, regardless the size, should be treated to avert further limb threatening events.
Duplex scan imaging is the first line imaging modality for the diagnosis and assessment of PAAs.
Treatment options include open bypass surgery and minimally invasive endovascular stent-grafting (if anatomically suitable).
Visceral and Renal Artery Aneurysms (VAAs) are rare and affect the main arteries supplying the circulation to the bowel, liver, spleen (celiac artery, superior mesenteric artery, and inferior mesenteric artery, and their branches) and to the kidneys (renal arteries).
The natural history of VAAs is not well understood as they are often non-symptomatic and found incidentally; however, they carry a risk of bursting/rupture that can result in life-threatening haemorrhage. The risk is higher when associated to inflammation/infection, connective disease disorders (i.e. Marfan syndrome, Ehlers–Danlos type IV or von Recklinghausen disease).
Asymptomatic aneurysms larger than 20–30 mm in diameter should be investigated for treatment. Treatment is indicated regardless of aneurysm size in splenic artery aneurysms diagnosed in pregnant women (due to the risk for the mother and the fetus), patients with portal hypertension and waiting for abdominal organ transplants.
Contrast-enhanced CT scan, magnetic resonance angiography, and abdominal ultrasound may help identify the morphology and features of the aneurysm, and thereby facilitate a definitive diagnosis.
Minimally invasive endovascular treatment, when feasible, is considered the first line treatment option with the view of excluding the aneurysm (hence preventing the risk of rupture) and preserving the blood flow to the organs.
Popliteal artery entrapment is a relatively rare condition in which an anatomical variant of the calf muscle (medial head of gastrocnemius) exerts pressure on the main artery behind the knee (popliteal artery). The artery becomes trapped, causing a functional impairment of the circulation to the lower leg and foot.
It is more prevalent in young and middle-aged athletes and may present as “intermittent claudication” (pain in the leg induced by exercise) or positional (prolonged plantar flexion) ischaemic pain.
In the long term, the repeated compression and trauma on the vessel may result in permanent arterial damage and blockage, ultimately threatening the viability of the lower limb.
Vascular assessment and dynamic Duplex investigations are necessary to reach a correct differential diagnosis and to address the appropriate surgical management.
Raynaud manifests as recurrent vasospasm of the digital arteries and pre-capillary arterioles of the fingers and toes; it usually occurs in response to stress or cold exposure.
Typically, the fingers change colour in the sequence white-blue-red (“French flag sign”): the white stage (ischemia) is due to excessive vasoconstriction and cessation of blood flow in the extremities; this is followed by a cyanotic phase (blue deoxygenation); the red phase (reperfusion) is due to blood flow restoration.
Raynaud’s phenomenon can be classified as primary (Raynaud’s Disease) or secondary (Raynaud ’s Phenomenon), depending on whether it occurs as an isolated condition or is associated mainly with a connective tissue disease (i.e. autoimmune conditions, connective tissue disorders, occupational factors, repetitive trauma, malignancies, clotting disease, neurodegenerative cause, nervous system diseases, endocrine diseases).
Reynaud disease is usually benign; the prognosis for patients with primary Raynaud disease is usually very good. In very rare cases, however, prolonged and recurrent ischemia of the digits can result in excruciating pain and skin damage (necrosis). Vascular assessment of the main arterial tree (with the view of ruling out inflow impairment) and Rheumatology review are paramount.
OPENING HOURS
| Monday – Friday | 8:00 – 17:00 |
| Saturday | 9:00 – 12:00 |
| Sunday | – |
