Peripheral Arterial Disease
The arteries carry oxygenated, high-pressure blood and nourishment from the heart to the organs and tissues of the body.
The Aorta represents the main trunk of the “arterial tree”, originating from the left ventricle of the heart; the main distribution branches in the pelvis and lower limbs are named iliac, common femoral, profunda femoris, superficial femoral, popliteal and tibial arteries reaching the foot.
In healthy, elastic vessels the arterial pulse can be felt over the arteries when lying near the surface of the skin as the result of the pumping action of the heart.
A blockage in the peripheral arteries may lead to a dramatic deterioration of the blood supply, affecting the nerves, muscles and skin of the limbs. This may occur as a sudden event (acute ischaemia) or as a chronic build-up of fat, cholesterol, platelets (“atheromatous plaque”) slowly narrowing the arterial lumen (peripheral arterial disease – PAD) progressively reducing the blood flow and pressure until reaching a complete, irreversible blockage.
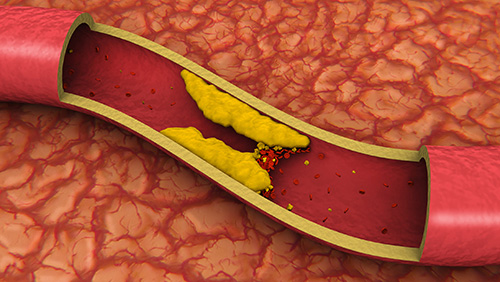
Smoking, high blood pressure, high cholesterol are some of the predisposing conditions that can be reduced with life-style modification and best medical therapy; male gender, age and genetic predisposition are unfortunately non-modifiable risk factors.
Classification
PAD may present with a wide spectrum of signs and symptoms:
- intermittent claudication: leg muscles cramp-like pain that triggers when walking a certain distance (the etymology of the name “claudication” comes from the ancient Roman emperor Claudius who reportedly was limping)
- rest pain: constant, debilitating leg pain; often keeps you awake at night-time. The only relief is to hang your leg off the bed or to sleep on the chair
- leg ulcerations: non-healing, arterial ulcers; these are prone to get infected and to evolve into a limb-threatening gangrene
Intermittent claudication (IC) is often a benign condition and the first-line management should be conservative by means of structured walking exercise and secondary cardiovascular risk factors modification. However, IC may sometimes progress into severely impairing walking limitations affecting the overall physical and psychological well-being.

A thorough vascular assessment is paramount to reach a correct differential diagnosis which should include:
- arterial claudication
- venous claudication
- neurological claudication
- muscle and joint claudication (musculoskeletal)
Ischaemic rest pain and foot-leg ulcerations are severe limb-threatening conditions (often referred as Critical Limb Ischaemia – CLI); timely diagnosis and intervention are indispensable to save the limbs from the risk of irreversible functional damages, life-threatening blood stream infections and limb loss.
The vascular assessment will comprise of:
- anamnesis (personal and medical history)
- comprehensive physical examination
- Doppler test (static or dynamic measurement of the pressure in the arteries of the leg)
- Ultrasound Duplex scan to investigate the anatomy of the vessels and to identify the extent and severity of the blockage or flow-limiting narrowing
- second level imaging (e.g. CTA, MRI) for differential diagnosis or surgical planning
Medical and Surgical management (according to the stage and anatomical distribution of the disease):
- life style recommendations
It is important to consider your lifestyle as part of your overall treatment plan to help support prevention, optimal treatment outcomes and recovery, and avert recurrences.
We are here to support and discuss with you how this may impact on your health and the overall benefits to your wellbeing.
Areas to consider:
- Diet and how it can be optimised to reduced lipid intake
- Exercise and how to improve joint and muscle functions and to promote collateral circulation
- Skin and nail care
- Footwear
- Smoking cessation strategies
- structured walking exercise programme (for IC)
- best medical therapy – medications
- minimally invasive “key-hole” endovascular treatment
- angioplasty and stenting (drilling through the plaque and stretching open a channel in the blocked arteries)
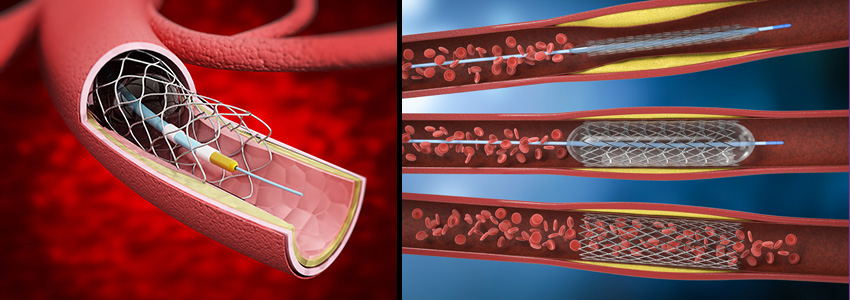
- atherectomy and shockwave intravascular lithotripsy (cutting edge technologies to debulk the plaque and to re-open heavily calcified, hardened arteries without the need of permanent metal stents)
- angioplasty and stenting (drilling through the plaque and stretching open a channel in the blocked arteries)
- open bypass surgery
- using a superficial vein as a conduit to bypass the blockage
- durable and preferable in young, fit patients
- hybrid procedures
- the combination of concomitant open surgery and endovascular therapy, performed in the state-of-the-art “hybrid theatre”. If suitable, this approach may offer the best outcomes
Surgical and endovascular treatments requires a close ultrasound and clinical surveillance, together with strict adherence to individualised medication strategies in order to optimise long-term results
OPENING HOURS
| Monday – Friday | 8:00 – 17:00 |
| Saturday | 9:00 – 12:00 |
| Sunday | – |
