Varicose Veins & Venous Insufficiency
Our legs and feet work really hard throughout our life: getting us up in the morning, bringing us to work every day, standing while cooking, walking up the mountains or through that gym class. Without the health of the blood vessels, we would find our lives less active, our mobility considerably reduced and possibly experience pain or limb-threatening conditions. Problems with the vessels in the lower leg can happen at any age but are more common at more mature stages of our lives.
To help prevent conditions of the lower limb vessels and treat current complaints it’s helpful to first understand what are the main vessels in the legs, how do they work and what happens when they become damaged and no longer work as they should.
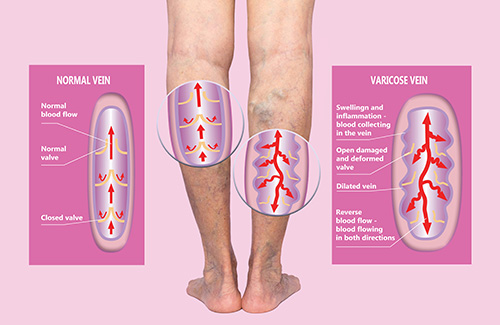
The venous system is a complex network of superficial and deep veins in which deoxygenated blood is conveyed from the periphery to the heart. This is a low-pressure system that relies on venous valves and muscle contraction (foot dorsi-flexion and calf muscle pump) to return blood to the heart against the gravity.
The Long (or Great) Saphenous – LSV and the Short Saphenous Vein – SSV are the main superficial veins of the legs; the Anterior Thigh Vein, the Giacomini and the Intersaphenous Veins are also important tributaries. The superficial veins drain into the deep venous system via junctions in the groin (sapheno-femoral) and behind the knee (sapheno-popliteal) and small perforator veins crossing the muscles.
Varicose veins are chronically dilated and tortuous superficial veins with reversed blood flow due to incompetent damaged valves and/or diseased venous wall. The stasis of the blood (venous hypertension) in the lower extremities may lead to chronic swelling, skin changes (pigmentation, eczema) and ultimately the risk of developing ulcerations. Often varicose vein may bleed or cause localised painful inflammatory process (phlebitis).
Risk factors for developing varicose veins include predisposition/family history, previous injuries, fractures or deep vein thrombosis – DVT (post thrombotic syndrome). The prevalence rises with age and often develop or deteriorate during pregnancy.
You may be have an increased risk of developing varicose veins if:
- You are pregnant or have had multiple pregnancies
- Stand for long periods of time at work or have a sedentary life-style
- Are overweight for your height
- Have reduced movement or ankle joint or calf muscle waist
- Have a family history of varicose veins
Stages of Venous Disease
- Spider Veins
Spider veins or Telangiectasia are tiny, dilated blood vessel capillaries arising from a central point therefore resembling a spider web. They can occur near the surface of the skin. Spider veins can be perceived as a cosmetic condition and have no clinical implication;

- Reticular Veins
Reticular veins are varicosities 1-3 mm in diameter; they can be an early sign of venous disease and it is useful to have them checked out along with any other symptoms you may be experiencing in your legs such as:
- pain, itchiness, leg heaviness
- skin changes such as dark, brownish pigmentation or eczema
It is reassuring to note that if the early sign of venous disease are addressed in the proper way it can prevent further complications later in life.

- Truncal Varicose Veins
Varicose veins 4mm or larger are defined as truncal; these are usually involving the long or short saphenous veins and the main tributaries. Truncal reflux may lead to venous hypertension and is associated to the risk of developing venous leg ulcers

- Oedema
More commonly known as swelling, it is usually located at the ankles, feet or legs. Oedema is a build-up of fluid. This can be very uncomfortable and may leave your legs feeling heavy and in some cases aching. It is important to investigate whether incompetent veins or lymphatic vessels (often a combination of the two) are causing the congestion. The good news is that venous-lymphatic oedema can be alleviated by appropriate support stockings/socks or compression hosiery and with elevation, rest and lifestyle advice
- Pigmentation or eczema
Haemosiderin staining is a typical clinical sign that you may have moderate to severe venous insufficiency. This is easy to recognise and to check yourself.
Usually located on the lower part of the leg or possibly the ankle, venous staining often presents as a notably brown, rusty yellow or black skin discolouration. This happens when the haemoglobin in the red blood cells leak out of the superficial veins as the result of the venous stasis.
It is usually not painful but can make the skin drier, frailer more susceptible to breakdown and possibly ulceration.

- Lipodermatosclerosis or athrophie blanche
Lipodermatosclerosis or athrophie blancheis is a form of chronic inflammation of the fat under the skin resulting into thickening, hardening and colour changes of the skin.
- Healed venous ulcer
C5 in the CEAP classification of chronic venous disease (link with photo). The risk of recurrences is extremely high unless the underlying venous hypertension is treated.
- Active venous ulcer
An active venous ulcer is classified as C6 in the CEAP classification of chronic venous disease (link with photo). Leg ulcer are a physical, psychological and economic burden. They may impact on your personal and social life. The correct treatment should include a holistic management by means of:
- appropriate wound care
- compression therapy
- surgical or endovenous treatment of the underlying truncal reflux
Management
The management of varicose veins, depending on the stage of the disease, your anatomy and your personal preference (following thorough informed discussion) may include:
- lifestyle recommendations and skin care
- Maintaining a healthy weight
- Eating a well-balanced and healthy diet
- Exercising
- Moving – if you sit or stand for long periods of time make sure to get up and move regularly
- Elevating your feet and legs above heart level – this can have a real soothing effect after a long day
- looking after and moisturising your skin
- interventional treatments of the varicose veins
- “key hole”, minimally invasive, endothermal ablation (radiofrequency – RFA)
- ultrasound guided foam sclerotherapy
- surgical avulsions and/or ligations of perforator veins
- fitted or customised compression hosiery
- Wearing fitted or customised compression hosiery or socks/stockings to support your veins
- the appropriate combination of the above
When attending the Vascular Clinic, a comprehensive anamnesis (personal and medical history) and a physical examination will be performed.
A duplex ultrasound scan may be arranged to further investigate the deep and superficial venous systems, the level of venous reflux and to map your varicose veins with the view of identifying the most suitable treatment strategy.
Mr Biasi will discuss with you how well each treatment is likely to work and the possible limitations or side effects.
If neither endothermal ablation nor ultrasound-guided foam sclerotherapy are suitable for you, you should be offered surgery. This is usually a type of surgery called ligation and stripping, in which the varicose vein is tied off and then removed

Thermal Ablation

Surgical Avulsions
Thermal Ablation (varicose vein treatment)
Sclerotherapy effectively treats spider veins
OPENING HOURS
| Monday – Friday | 8:00 – 17:00 |
| Saturday | 9:00 – 12:00 |
| Sunday | – |
